When I first started looking closely at Ozempic, I was struck by how many people are curious about both its benefits and its downsides. Ozempic is a medication used to manage type 2 diabetes, and it does a strong job helping to control blood sugar — but it also comes with a list of potential side effects that every patient should understand.
Figuring out how long Ozempic side effects last matters because the timeline affects how you live day to day and how your doctor and I might adjust your treatment. Experiences vary: some people breeze through the adjustment period, while others deal with symptoms longer. In this piece I’ll walk you through the common side effects, what I’ve seen in practice, and the timelines you can reasonably expect based on the evidence.
My goal here is practical: to help you make an informed choice about your health by explaining the likely side effects and when they usually resolve. If anything in this article raises questions for you, please get in touch with your doctor — and remember this is general guidance, not individualized medical advice.
Key Takeaways
- Ozempic is a medication used to manage type 2 diabetes.
- Common side effects may occur, and their duration varies from person to person.
- Understanding possible side effects helps you and your care team make better decisions.
- Everyone’s experience with Ozempic side effects can be different, so tracking symptoms is useful.
- The information below is grounded in credible sources and my clinical observations about health and patient care.
Understanding Ozempic: What It Is and How It Works
Let me start by saying I view Ozempic as a powerful tool with specific uses and limits. Ozempic (semaglutide) was developed to treat type 2 diabetes, and in that role it helps people lower their blood sugar reliably. Along the way, clinicians noticed it often produces significant weight loss, which is why it’s become so widely discussed.
The Rise of Ozempic for Weight Loss
In studies and in clinic, Ozempic has repeatedly shown meaningful weight reduction for many people. That outcome comes from the drug’s action on appetite and food intake — in plain terms, it helps many patients feel less hungry and eat less. Because of those results, people without diabetes sometimes seek Ozempic for weight management, but that’s an important distinction to keep in mind.
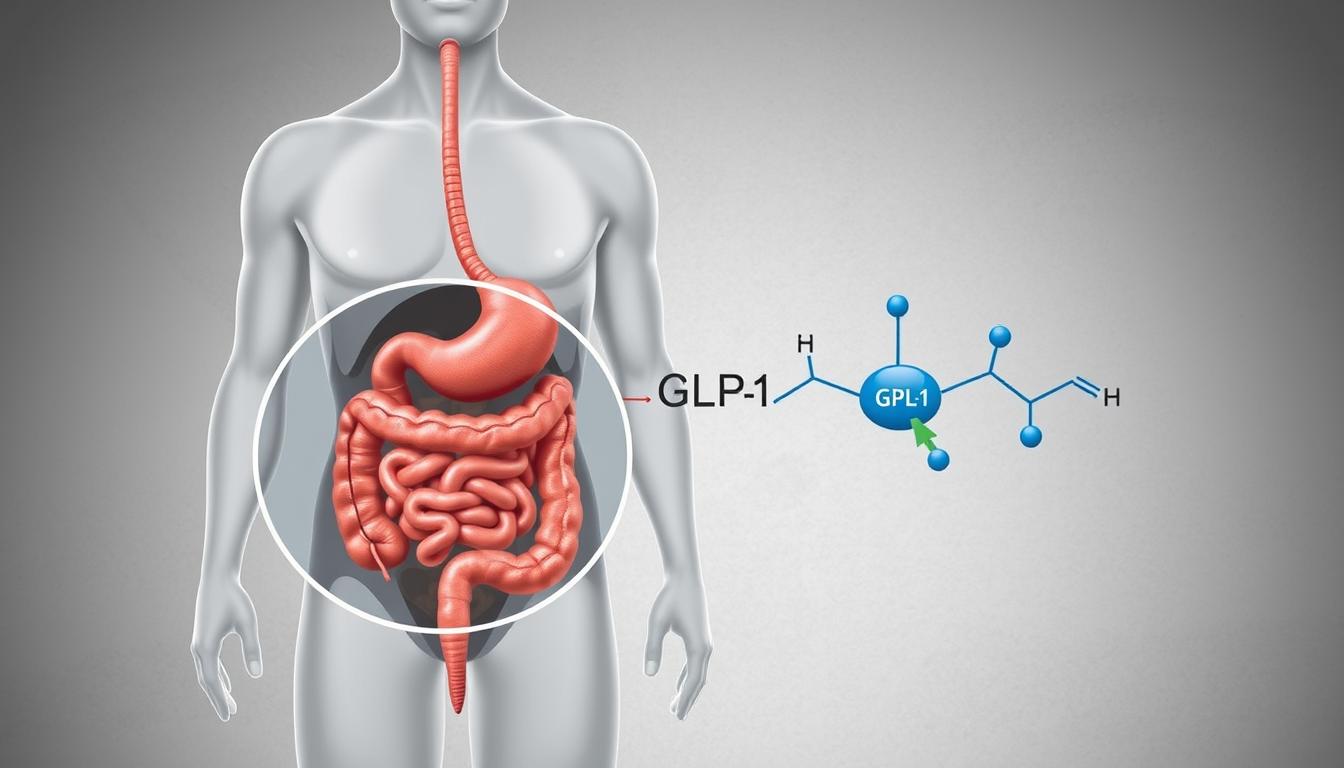
GLP-1 Mechanism of Action
I explain the mechanism like this to patients: Ozempic acts like the GLP-1 hormone your body uses to regulate glucose and appetite. As a GLP-1 receptor agonist, it does three clinically important things — it boosts insulin release when glucose is high, it reduces glucagon secretion, and it slows gastric emptying. Together, those effects help stabilize blood sugar and reduce how quickly you feel hungry after a meal.
FDA-Approved Uses vs. Off-Label Prescribing
Here’s the practical takeaway I give patients: Ozempic is FDA-approved for managing type 2 diabetes. Using Ozempic specifically for weight loss is generally considered off-label — the higher-dose semaglutide formulation branded as Wegovy is the one FDA-approved for chronic weight management. The table below summarizes that difference and the typical dosing context.
| UseStatusDosage | ||
| Type 2 Diabetes Management | FDA-Approved | Ozempic (semaglutide) |
| Weight Loss | Off-Label (Ozempic), FDA-Approved (Wegovy) | Ozempic (lower dose), Wegovy (higher dose) |
In my practice I stress discussing the intended use with your doctor before starting semaglutide for weight goals. Clinical trial data and the FDA label are good sources for understanding benefits and risks; if you want, I can point you toward those references so you can review the primary evidence before seeking medical advice.
Common Side Effects of Ozempic
I tell patients up front that Ozempic can cause a range of side effects — many are annoying but temporary, and some are less common and more serious. Understanding what to expect helps you stick with treatment when appropriate and recognize when to seek help.
Gastrointestinal Side Effects
The most frequent issues people report are gastrointestinal. Typical complaints include:
- Nausea
- Vomiting
- Diarrhea
- Abdominal pain
- Constipation
Because Ozempic slows gastric emptying, it’s common to feel full or uncomfortable after meals. In my experience, nausea is the single most commonly reported symptom and often improves after a few weeks once the dose is tolerated. Practical tips I give patients: eat smaller, more frequent meals, choose bland low-fat foods when queasy, and avoid rich or very greasy meals until tolerance improves.
Systemic Side Effects
Beyond the stomach, some people notice systemic effects such as:
- Fatigue
- Dizziness
- Headaches
These can interfere with daily life, so I advise tracking symptom severity and timing — that information helps your clinician decide whether to adjust the dose or try different strategies to manage symptoms.
Rare but Serious Adverse Reactions
While less common, there are serious risks worth knowing about. These include:
- Pancreatitis
- Thyroid C‑cell tumors (observed in rodent studies; human risk is uncertain)
- Allergic reactions
“The risk of pancreatitis is a concern for many of my patients on Ozempic. It’s a reminder of the importance of careful patient selection and monitoring.”
If you experience severe abdominal pain, persistent vomiting, signs of allergic reaction (swelling, difficulty breathing), or sudden worsening symptoms, contact your doctor right away — these can be signs of serious side effects. Overall, being informed and proactive helps you and your care team balance the benefits and risks of treatment.
How Long Does Ozempic Side Effects Last? The Timeline Explained
A question I hear all the time is: how long do Ozempic side effects last? From my experience and the clinical data, the answer depends on which side effect you’re looking at and how your body responds. Below I outline a practical timeline I share with patients so you know what to expect and when to call your doctor.
Initial Adjustment Period (First 4 Weeks)
In the first few weeks—typically the 0–4 week window—most people experience the brunt of gastrointestinal symptoms. Common complaints include nausea, vomiting, diarrhea, and abdominal pain. For many, these side effects are mild-to-moderate and begin to fade after 2–4 weeks as the body adjusts to the medication.
Why that happens: semaglutide slows stomach emptying and alters appetite signals, so the GI tract needs time to adapt. Because of the drug’s pharmacology, some symptoms may linger a bit longer than with short-acting drugs.
Medium-Term Side Effects (1-3 Months)
Between 1 and 3 months, the picture often improves for GI complaints, but other issues may appear or persist — for example, injection-site reactions, fatigue, and dizziness. If you’re on other glucose-lowering medicines, pay attention to your blood sugar levels during this time: changes in appetite or weight can affect glucose control and, in rare cases, contribute to episodes of low blood sugar.
Long-Term Side Effect Considerations
With longer use, some risks that are rare but serious come into view. These include pancreatitis, thyroid C-cell concerns, and, in isolated reports, kidney injury. Because these are less common yet potentially serious side effects, I advise regular follow-up with your healthcare team and prompt reporting of worrying signs.
| TimeframeCommon Side EffectsSerious Side Effects | ||
| Initial (0-4 weeks) | Nausea, vomiting, diarrhea, abdominal pain | Rare |
| Medium-term (1-3 months) | Injection site reactions, fatigue, dizziness | Pancreatitis, thyroid issues |
| Long-term | Varies, may include gastrointestinal issues | Acute kidney injury, thyroid C-cell tumors |
Practical checklist I give patients during each phase:
- Initial (0–4 weeks): keep a symptom log (what you ate, nausea timing), stay hydrated, eat small frequent meals, and avoid high-fat foods.
- Medium-term (1–3 months): monitor blood sugar more closely if you’re on insulin or sulfonylureas and report persistent fatigue or dizziness.
- Long-term: schedule routine follow-ups so your clinician can watch for rare but serious complications.
If you notice severe abdominal pain, persistent vomiting, signs of dehydration, very low or high blood glucose, or any sudden concerning change, call your doctor immediately—these can be red flags for serious side effects. Overall, knowing the typical timelines for how long side effects tend to last helps you set expectations and stay in control of your care.
Case Studies: Real Patient Experiences with Ozempic Side Effects
I often share real-world examples with patients because they make abstract risks and timelines easier to grasp. Below are three illustrative stories I’ve seen or heard about — they aren’t statistics, but they do reflect the range of ways people respond to Ozempic (semaglutide).
Patient Profile: Short-Term Side Effect Resolution
A 45-year-old woman with type 2 diabetes started Ozempic at 0.5 mg weekly. She experienced nausea and stomach discomfort during the first few weeks, but those symptoms faded after about a month as her body adjusted.
By month two, her blood sugar improved noticeably and the remaining side effects were minimal. Takeaway: gradual titration and patience can pay off — if symptoms are tolerable, many people see improvement and continue treatment successfully.
Patient Profile: Persistent Side Effects
A 35-year-old man used Ozempic primarily for weight loss. He began at 0.25 mg and increased slowly, but continued to have stomach upset and diarrhea for six months. In his case the side effects were persistent enough that he and his doctor discussed alternative strategies.
Takeaway: not everyone tolerates the medication long-term; when side effects persist, it’s reasonable to re-evaluate dosing or consider other options.
Patient Profile: Side Effects After Discontinuation
A 50-year-old woman had been on Ozempic for over a year for weight control but stopped because of ongoing GI issues. After stopping, she noticed increased appetite and what felt like withdrawal-like symptoms — hunger returned and mood shifted for a few weeks. Over the following couple of months she gradually returned to baseline.
Takeaway: stopping Ozempic can bring rebound effects for some people, so I recommend planning discontinuation with your care team and monitoring your response.
What I want you to take away from these stories is simple: individual experiences with Ozempic side effects vary. Track your symptoms, share that log with your doctor, and treat these examples as conversation starters with your care team when deciding whether to continue, change, or stop treatment.
Factors That Influence the Duration of Ozempic Side Effects
From my clinical experience, there’s no single answer to how long Ozempic side effects last — the length depends a lot on a few predictable factors. If you understand these, you and your doctor can make smarter choices about starting, titrating, or stopping treatment.
Dosage and Titration Schedule
I always advise a gradual titration because it genuinely reduces the chance and severity of early side effects. The usual approach starts with a low dose for a few weeks (for example, 0.25 mg weekly for about four weeks) before increasing to 0.5 mg weekly; clinicians may then adjust based on response and tolerability. Moving slowly gives your body time to adapt and often shortens how long GI symptoms last.
Individual Physiological Differences
Each person metabolizes medications differently. Age, kidney function, and even genetic factors can change how long semaglutide stays in your system and how intensely you feel effects. In particular, people with reduced renal function may clear drugs more slowly and experience prolonged symptoms, so personalized monitoring is important.
Concurrent Medications and Conditions
What else you take and what health conditions you have matter a lot. If you’re on other glucose-lowering drugs (insulin, sulfonylureas), changes in appetite or weight can affect your blood sugar control and raise the risk of low blood sugar. Gastrointestinal disorders may amplify GI side effects, and certain medications can interact to make symptoms worse or last longer.
| FactorInfluence on Ozempic Side Effects | |
| Titration & Timing (weeks) | Slower increases usually reduce early GI side effects |
| Individual physiology | Age, renal function, genetics can prolong or shorten symptom duration |
| Other meds & conditions | Drug interactions and preexisting GI or metabolic conditions can extend side effects |
Practical tip I give patients: before you start or change an Ozempic regimen, list all your current medications and any ongoing conditions and discuss them with your doctor. That simple step helps tailor care and reduce surprises during treatment.
Managing and Reducing Ozempic Side Effects
From my conversations with patients, practical steps make a big difference in how tolerable Ozempic is. While the drug is used for type 2 diabetes and can help with weight loss, small lifestyle and dietary changes often reduce the intensity and frequency of unwanted side effects.
Dietary Modifications That Help
I usually recommend these simple food strategies when GI symptoms start:
- Eat smaller, more frequent meals rather than three large ones — this often eases nausea and stomach discomfort.
- Choose bland, low-fat options when you feel queasy: plain toast, rice, applesauce, bananas, or broth.
- Favor high-fiber foods (fruits, vegetables, whole grains) to help regulate digestion, but introduce fiber slowly if you’re also dealing with diarrhea or bloating.
- Avoid very greasy, spicy, or sugary foods in the early weeks to minimize upset.
These are practical, low-risk adjustments that many people find helpful while their bodies adapt.
Hydration and Lifestyle Adjustments
Staying well-hydrated is one of the easiest ways to reduce problems like headaches, dizziness, and symptoms linked to dehydration. I tell patients to aim for regular fluids throughout the day — not just a single large amount — and to pay attention to urine color as a quick check (pale is better).
Regular gentle activity, like walking, supports digestion and health generally. I also advise limiting alcohol and avoiding smoking, both of which can worsen GI symptoms and overall tolerance.
| Lifestyle AdjustmentBenefit | |
| Eating smaller, frequent meals | Reduces gastrointestinal side effects like nausea and vomiting |
| Staying hydrated | Prevents dehydration and reduces headache and dizziness |
| Regular physical activity | Improves overall health and may help manage weight and stress |
When to Consult Your Healthcare Provider
While many side effects can be managed at home, certain signs need prompt attention. Contact your doctor right away if you have:
- Severe or persistent abdominal pain (possible pancreatitis)
- Ongoing vomiting or inability to keep fluids down
- Symptoms of dehydration (very low urine output, lightheadedness)
- Very low or very high blood sugars, especially if you’re on insulin or sulfonylureas
Your healthcare team can provide individualized care: adjust the dose, change the titration schedule, or recommend alternative treatments if necessary. I also encourage keeping a short symptom log (what you ate, timing of nausea, hydration status) to bring to visits — it makes dose decisions and follow-up far more effective.
Side Effects After Stopping Ozempic
In my practice I always tell people that stopping Ozempic deserves a plan — you can still experience side effects after discontinuation, and how your body responds matters for weeks.
The Half-Life of Semaglutide
Semaglutide (the active ingredient in Ozempic) has a relatively long elimination time: its half-life is roughly one week, which means the drug can take around five weeks to clear from the system. That pharmacology helps explain why some side effects can hang around for several weeks after the last dose.
Withdrawal Symptoms vs. Rebound Effects
When people stop Ozempic, two patterns can occur. First, some experience transient withdrawal symptoms as their body readjusts — common examples are nausea and headaches. Second, rebound effects can emerge, where previous issues return or worsen, such as rising blood sugar or weight gain.
- Common withdrawal symptoms: nausea, headaches, and temporary changes in appetite.
- Possible rebound effects: return of higher blood glucose readings or regain of lost weight.
Timeline for Body Normalization
Generally, many people begin to feel more like themselves within a few weeks, but individual responses vary. If you’re on insulin or sulfonylureas, stopping Ozempic without coordinating with your doctor can raise the risk of low blood sugar or unpredictable glucose swings — so plan ahead.
My practical advice: don’t stop abruptly without a clinician’s input, monitor your symptoms and blood sugars closely for several weeks after stopping, and schedule follow-up so your care team can help manage any lingering or rebound effects.
The Hidden Costs: Long-Term Implications of Ozempic Use
I’m cautious about presenting Ozempic as a quick fix — yes, it can drive substantial weight loss, but there are longer-term considerations I talk through with patients before we commit to prolonged use.
Potential Impact on Gut Microbiome
The gut microbiome plays a big role in digestion, immunity, and metabolism. Early studies suggest semaglutide may alter gut microbial composition, which may also have downstream effects on metabolism and overall health. The human evidence is still emerging, so I frame this as a possible risk rather than a proven outcome.
Muscle Mass Concerns
Another issue I watch for is loss of muscle during rapid weight reduction. Because GLP‑1 receptor agonists like Ozempic reduce appetite, people who aren’t careful about protein intake and resistance exercise can lose lean mass. Less muscle can slow metabolic rate and make long-term weight maintenance harder.
Practical mitigation I recommend: include resistance training and adequate protein in your routine to help preserve muscle while losing fat.
Psychological Dependence and Weight Management
From a behavioral perspective, I’ve seen people become reliant on the medication to control their weight, sometimes at the expense of building sustainable lifestyle habits. That psychological dependence isn’t a formal diagnosis, but it’s a real challenge: when the drug stops, habits aren’t always in place to keep the weight off.
The Rebound Weight Gain Phenomenon
Rebound weight gain after stopping Ozempic is a genuine concern. Many people regain some or all of the weight they lost — and occasionally more — which can be demoralizing. That’s why I emphasize planning for transitions off medication with a clear strategy: dietary, activity, and behavioral supports, plus close follow-up with your doctor.
In short, while Ozempic can be a highly effective tool for weight loss and diabetes management, the potential long-term effects and risks mean it should be part of a broader plan that includes exercise, nutrition, and psychological supports. Discuss these trade-offs with your care team so you aren’t surprised down the line.
Conclusion: Weighing the Benefits Against Side Effect Duration
My bottom line: Ozempic can be a very effective medication for managing diabetes and supporting weight loss, but it isn’t a one-size-fits-all solution. Like any drug, it brings potential side effects that vary in intensity and how long they last. Deciding whether the benefits outweigh the risks is a personal judgment best made with your doctor and care team.
How long side effects stick around depends on several things — dose and titration speed, your individual physiology, other medications you take, and how closely you and your care team monitor symptoms and blood glucose levels. For many people, the most bothersome symptoms improve within a few weeks, but some effects may take longer or require treatment changes.
Here’s what I recommend based on what I’ve seen work in practice: keep a brief symptom log (what you ate, when symptoms happen), check blood sugars if you’re on glucose‑lowering therapies, and schedule regular follow-up so your clinician can adjust dose or strategy as needed. If anything feels severe or sudden, contact your doctor right away — this is not just general information but guidance about safety and monitoring.
FAQ
How long do Ozempic side effects typically last?
They can last from a few weeks to several months depending on the symptom and the individual. Early gastrointestinal symptoms commonly improve within 2–4 weeks, while other effects may persist longer.
What are the most common side effects of Ozempic?
The most common complaints are nausea, vomiting, and diarrhea; fatigue and headache are also reported. Most are temporary, but track their severity and duration.
How long do Ozempic side effects last after stopping the medication?
Because semaglutide has a long elimination time, some effects can continue for several weeks after stopping. You may see temporary withdrawal-like symptoms and possible rebound in appetite or blood glucose; plan discontinuation with your provider.
Can dietary modifications help alleviate Ozempic side effects?
Yes—small, frequent meals, bland low‑fat choices during nausea, and steady hydration often help. Pair dietary steps with activity and protein to protect muscle during weight loss.
What factors influence the duration of Ozempic side effects?
Dosage and how quickly you titrate, your age and kidney function, concurrent medications, and baseline GI conditions all influence how long side effects last.
Are there any long-term implications of using Ozempic?
Long-term use may may also have implications for gut microbiome composition and muscle mass, and some people describe psychological reliance on the medication for weight control. These are reasons to include lifestyle and behavioral supports alongside drug therapy.
How long does it take for the body to normalize after stopping Ozempic?
Normalization varies but often occurs over several weeks as the drug clears. If you’re on insulin or sulfonylureas, expect careful monitoring because glucose can change unpredictably.
Can Ozempic side effects be persistent?
While many side effects resolve, some can persist and require dose adjustments or alternative therapies. Work closely with your clinician to manage persistent issues and get tailored medical advice.
What about diabetic eye disease (diabetic retinopathy) concerns?
Rapid improvements in glucose control can sometimes unmask or temporarily worsen diabetic retinopathy in susceptible patients; discuss eye monitoring with your doctor if you have long-standing diabetes.